The statistics are sobering. Over 1/3rd of us are obese. In 2012, The London School of Hygiene and Tropical Medicine calculated the average Body Mass Index for 177 countries, and America was in the top 5 with an average Body Mass Index of 27.82 (behind Tonga, Micronesia, Croatia and Greece).
From the Centers for Disease Control:
69.2% of adults over 20 years old are either overweight or obese
35.9% of adults over 20 years old are obese
41.8% of 60- to 74-year-old males are obese
36.9% of 60- to 74-year-old women are obese
According to the National Health and Nutrition Examination Survey (NHANES), the average male weighed 166.3 lbs in 1960, and by 2002 he weighed 191 lbs, an increase of nearly 25 lbs. The average female weighed 140 lbs in 1960, and by 2002 she weighed 164.3 lbs. Thus, we live in a country with heavy citizens and one in which, over the past half century, its citizens have become heavier. As they age, they become heavier still.
According to the CDC, obesity is associated with coronary heart disease, type 2 diabetes, hypertension, cancers of the endometrium, breast and colon, dyslipidemia, stroke, sleep apnea, liver and gallbladder disease and gynecological problems such as abnormal menses and infertility. It is associated with medical costs of $150 billion dollars, or 10% of the medical budget. The center has a good video segment on it
here
Many Americans don’t realize they are overweight or obese. Harris Interactive performed a
poll, and 30% of overweight individuals thought they were normal weight, and 70% of obese individuals felt they were simply overweight. As stated in an earlier blog post, from a medical perspective, obesity is defined by the body mass index (BMI). A BMI of 30 is obese, while a body mass index greater than 25 is overweight. The body mass index was created by Adolphe Quetelet in the 1800s, was advanced by the epidemiologist Ancel Keys in the 1970s, and has been used for population studies for decades.
A visual representation of the Body Mass Index is seen in this chart below:
To use this chart, find your height on the left and your weight on the top and then determine your body mass index. Determine your BMI with minimal clothes and no shoes. A healthy body mass index is considered from 18.5 to 24.9, overweight from 25 to 29.9 and obesity from 30 onwards. A BMI
calculator is also located online from the National Heart Lung and Blood institute.
As a simple epidemiological tool, it can give a good deal of information about groups, as higher BMIs are associated with increasing risk of certain disease states, particularly diabetes. The Harvard School Department of Public Health sent out screening questionnaires to over 51,529 U.S. male health care providers over a 5 year period of time. They also analyzed the data from over 114,000 female nurses. As can be seen by the graph below, BMI strongly correlated with the risk of developing diabetes, particularly for women. Even women in the "healthy BMI range" still had a substantially increased risk of developing diabetes if their body mass index was 24 instead of 21.
 |
| Adapted from Colditz GA, Willett WC, Rotnitzky A, Manson JE. Weight gain as a risk factor for clinical diabetes mellitus in women. Ann Intern Med 1995;122:481-486; and Chan JM, Rimm EB, Colditz GA, et al. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care 1994;17:961-969. |
Other weight scales have been used in the past. For instance, in 1942 Louis Dublin, a statistician working with Metlife, examined the mortality and weight of 4 million Metlife subscribers and developed a Desirable Body Weight for men and women. He divided people up into Small, Medium and Large frame based on their skeletal structure. He determined the skeletal size based on the size of the elbow, but you could also estimate skeletal size by wrapping your right thumb and middle finger around your left wrist. If your thumb overlaps your middle finger, you are small frame, if they just touch then you have a medium frame, and if they don't touch, you are large frame. His scale was determined with his subjects wearing shoes and 3 lbs of clothes. For the most part, his desirable body weights seem thinner, around a BMI of 21-23. The major criticism of the Desirable Body Weight Scale came from a gentleman named Andres, who stated that it may be a good scale for individuals, but as people aged, more weight may actually be protective from a health standpoint.
1986 Met Life Desirable Body Weight for Women
1986 Met Life Desirable Body Weight for Men
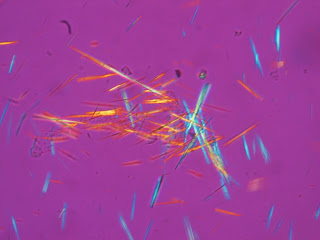
Overall, the BMI may be a useful tool to estimate an individual's or country's risk for certain disease states. However, there are potential limitations of the BMI. The BMI does not take into account several factors, such as one's gender, nationality, body composition (such as waist circumference or lean body mass). Not all fat appears to be equal. The visceral fat, the fat in the abdominal cavity around the inner organs (such as the liver, the pancreas, the kidneys) appears to harbor much greater risk in terms of insulin resistance and future cardiac morbidity. Here is an MRI of abdomens of the same waist circumference, yet some individuals have more muscle mass, and some have a great deal more intra-abdominal adipose (fat) tissue -- the white stuff instead of the dense grey muscles.
 |
| (From Wikipedia) |
In regards to identify individuals at greatest risk, efforts to determine body fat composition have been undertaken.
The waist-hip circumference ratio is a bio-metric study to help determine this visceral adiposity. Here is a nice diagram from the International Chair on Cardiometabolic risk to measure one’s waist.
(They also have a good website at www.
myhealthywaist.org) The size of the hips is usually determined with both feet together and using a measuring tape around the largest part of the hips. For men, the Waist to Hip ratio should be less than 0.9, and for women, less than 0.85. An absolute waist circumference of 40 inches for men and 35 inches for women also puts individuals at risk for cardiovascular events.
Writing in the American Journal of Epidemiology, researchers determined that waist circumference was more predictive of coronary heart disease among middle aged and older US Men than the BMI alone.
Another concern regarding the BMI is differences across nationalities. In Japan, for instance, a BMI of 25 is considered obese by the Japanese Society of Obesity, secondary to the increased risk of diabetes in Japanese over a BMI of 25. In 2008, Japan instituted a
law for workplaces and governmental facilities to measure the waistlines of all adults aged 40 to 74. The cutoff was 33.5 inches for men and 35.4 inches for women. Honestly, how many white or black American males have waistlines less than 33.5 inches? In Silicon Valley, where many people are from South Asia, there is a South Asian Body Mass
Calculator created by Sutter Health, which defines healthy weight as a BMI of 18.5 to 23, overweight as a BMI of 23.1 to 25, and obesity as a BMI of > 25. They recommend any South Asian with a BMI over 23.1 to get screened for diabetes, hypertension and hypercholesterolemia. One of the major concerns for the increased rate of disease states at lower BMIs among certain ethnic groups is that they may be more prone to create this visceral fat and thus place them at higher risk of disease. In such cases, a waist to hip ratio may be more accurate in defining risk.
For its own definition of obesity, the American Council of
Exercise focuses on total body fat percentage. This is often determined with various measurements such as calipers or bioelectric impedance analysis, which sends a small current through the body to estimate total body fat. By their guidelines:
Description Women Men
Essential Fat 10-13% 2-5%
Athletes 14-20% 6-13%
Fitness 21-24% 14-17%
Acceptable 25-31% 18-24%
Obesity >32% >25%
So where does that leave us, dear reader? I truly think it depends on knowledge of your own risks. If you are from South Asia or India, a "normal" BMI may place you at significant risk for heart disease compared to a white American. If you are Denver Broncos Corner Back Tony Carter, you may have a BMI of 25.8, but your lean body mass is likely very high, so are you really overweight? While the average American male has gained nearly 25 lbs since 1960, he was much more likely to smoke in 1960, which makes it unlikely that the 1960s male was "healthier" than his counterpart in 2014. The weight we carry, in my opinion, requires awareness of our ethnicity, our waist-to-hip ratio, our waist circumference to help assess our own visceral adiposity and an honest assessment of our risks based on our blood sugar, cholesterol and blood pressure. And, honestly, most of us could stand to lose 5 to 10 lbs, and even such a small amount of weight loss can lead to reduced risks of many disease states.
If you like, you can even evaluate yourself on the London School of Hygiene and Tropical Medicine's Global Fat
Scale.
Sources for blog that don't have links (since I can not figure out footnotes...)